Heel Soreness
Overview
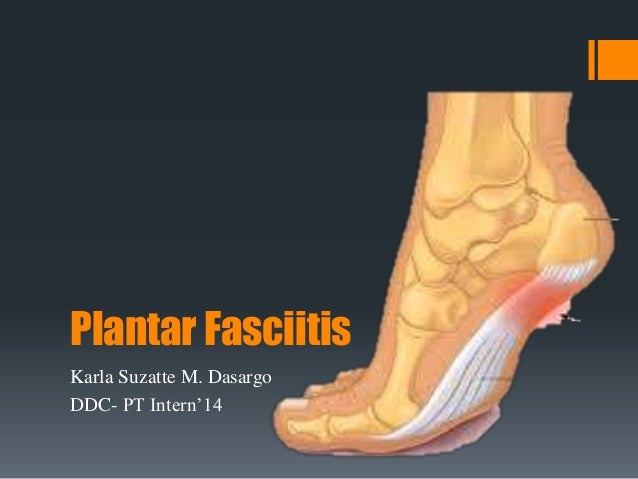
The most common cause of Heel Pain is plantar fasciitis which is commonly referred to as a heel spur. Plantar fascia is a broad band of fibrous tissue which runs along the bottom surface of the foot, from the heel to the toes. Plantar fasciitis is a condition in which the plantar fascia is inflamed. This condition can be very painful and cause a considerable amount of suffering.
Causes
Plantar fasciitis: It is the most common cause of heel pain. In this condition, the pain is more severe in the morning but becomes less painful as the day continues. It occurs due to tiny tears in the plantar fascia.The plantar faschia is a tissue band that connects the bottom of the heel bones to the ball of the foot and is involved in walking and running, giving spring to the step. If left untreated, the symptoms usually worsen and can lead to problems with the knee and hip and can cause back pain due to difficulty walking. Those who frequently stand or walk throughout the day or those who run are most likely to develop plantar fasciitis.
Symptoms
Pain in the heel can be caused by many things. The commonest cause is plantar fascitis. Other causes include, being overweight, constantly being on your feet, especially on a hard surface like concrete and wearing hard-soled footwear, thinning or weakness of the fat pads of the heel, injury to the bones or padding of the heel, arthritis in the ankle or heel (subtalar) joint, irritation of the nerves on the inner or outer sides of the heel, fracture of the heel bone (calcaneum).
Diagnosis
Your doctor will perform a physical exam and ask questions about your medical history and symptoms, such as have you had this type of heel pain before? When did your pain begin? Do you have pain upon your first steps in the morning or after your first steps after rest? Is the pain dull and aching or sharp and stabbing? Is it worse after exercise? Is it worse when standing? Did you fall or twist your ankle recently? Are you a runner? If so, how far and how often do you run? Do you walk or stand for long periods of time? What kind of shoes do you wear? Do you have any other symptoms? Your doctor may order a foot x-ray. You may need to see a physical therapist to learn exercises to stretch and strengthen your foot. Your doctor may recommend a night splint to help stretch your foot. Surgery may be recommended in some cases.
Non Surgical Treatment
Heel pain often goes away on its own with home care. For heel pain that isn't severe, try the following. Rest. If possible, avoid activities that put stress on your heels, such as running, standing for long periods or walking on hard surfaces. Ice. Place an ice pack or bag of frozen peas on your heel for 15 to 20 minutes three times a day. New shoes. Be sure your shoes fit properly and provide plenty of support. If you're an athlete, choose shoes appropriate for your sport and replace them regularly. Foot supports. Heel cups or wedges that you buy in the drugstore often provide relief. Custom-made orthotics usually aren't needed for heel problems. Over-the-counter pain medications. Aspirin or ibuprofen (Advil, Motrin IB, others) can reduce inflammation and pain.
Surgical Treatment
It is rare to need an operation for heel pain. It would only be offered if all simpler treatments have failed and, in particular, you are a reasonable weight for your height and the stresses on your heel cannot be improved by modifying your activities or footwear. The aim of an operation is to release part of the plantar fascia from the heel bone and reduce the tension in it. Many surgeons would also explore and free the small nerves on the inner side of your heel as these are sometimes trapped by bands of tight tissue. This sort of surgery can be done through a cut about 3cm long on the inner side of your heel. Recently there has been a lot of interest in doing the operation by keyhole surgery, but this has not yet been proven to be effective and safe. Most people who have an operation are better afterwards, but it can take months to get the benefit of the operation and the wound can take a while to heal fully. Tingling or numbness on the side of the heel may occur after operation.
Prevention

Wearing real good, supportive shoes are a great way to avoid heel pain. Usually, New Balance is a good shoe to wear, just for everyday shoe gear. By wearing proper footwear and performing thorough stretches, athletes can help prevent frequent heel pain. If you are starting to get a little discomfort or pain in the feet or heel, know that pain is not normal. So if you are having pain, you should be proactive and visit our office. If you let heel pain get out of control you could run into several other problems. It is always suggested to visit a podiatrist whenever you are experiencing pain.
The most common cause of Heel Pain is plantar fasciitis which is commonly referred to as a heel spur. Plantar fascia is a broad band of fibrous tissue which runs along the bottom surface of the foot, from the heel to the toes. Plantar fasciitis is a condition in which the plantar fascia is inflamed. This condition can be very painful and cause a considerable amount of suffering.
Causes
Plantar fasciitis: It is the most common cause of heel pain. In this condition, the pain is more severe in the morning but becomes less painful as the day continues. It occurs due to tiny tears in the plantar fascia.The plantar faschia is a tissue band that connects the bottom of the heel bones to the ball of the foot and is involved in walking and running, giving spring to the step. If left untreated, the symptoms usually worsen and can lead to problems with the knee and hip and can cause back pain due to difficulty walking. Those who frequently stand or walk throughout the day or those who run are most likely to develop plantar fasciitis.
Symptoms
Pain in the heel can be caused by many things. The commonest cause is plantar fascitis. Other causes include, being overweight, constantly being on your feet, especially on a hard surface like concrete and wearing hard-soled footwear, thinning or weakness of the fat pads of the heel, injury to the bones or padding of the heel, arthritis in the ankle or heel (subtalar) joint, irritation of the nerves on the inner or outer sides of the heel, fracture of the heel bone (calcaneum).
Diagnosis
Your doctor will perform a physical exam and ask questions about your medical history and symptoms, such as have you had this type of heel pain before? When did your pain begin? Do you have pain upon your first steps in the morning or after your first steps after rest? Is the pain dull and aching or sharp and stabbing? Is it worse after exercise? Is it worse when standing? Did you fall or twist your ankle recently? Are you a runner? If so, how far and how often do you run? Do you walk or stand for long periods of time? What kind of shoes do you wear? Do you have any other symptoms? Your doctor may order a foot x-ray. You may need to see a physical therapist to learn exercises to stretch and strengthen your foot. Your doctor may recommend a night splint to help stretch your foot. Surgery may be recommended in some cases.
Non Surgical Treatment
Heel pain often goes away on its own with home care. For heel pain that isn't severe, try the following. Rest. If possible, avoid activities that put stress on your heels, such as running, standing for long periods or walking on hard surfaces. Ice. Place an ice pack or bag of frozen peas on your heel for 15 to 20 minutes three times a day. New shoes. Be sure your shoes fit properly and provide plenty of support. If you're an athlete, choose shoes appropriate for your sport and replace them regularly. Foot supports. Heel cups or wedges that you buy in the drugstore often provide relief. Custom-made orthotics usually aren't needed for heel problems. Over-the-counter pain medications. Aspirin or ibuprofen (Advil, Motrin IB, others) can reduce inflammation and pain.
Surgical Treatment
It is rare to need an operation for heel pain. It would only be offered if all simpler treatments have failed and, in particular, you are a reasonable weight for your height and the stresses on your heel cannot be improved by modifying your activities or footwear. The aim of an operation is to release part of the plantar fascia from the heel bone and reduce the tension in it. Many surgeons would also explore and free the small nerves on the inner side of your heel as these are sometimes trapped by bands of tight tissue. This sort of surgery can be done through a cut about 3cm long on the inner side of your heel. Recently there has been a lot of interest in doing the operation by keyhole surgery, but this has not yet been proven to be effective and safe. Most people who have an operation are better afterwards, but it can take months to get the benefit of the operation and the wound can take a while to heal fully. Tingling or numbness on the side of the heel may occur after operation.
Prevention

Wearing real good, supportive shoes are a great way to avoid heel pain. Usually, New Balance is a good shoe to wear, just for everyday shoe gear. By wearing proper footwear and performing thorough stretches, athletes can help prevent frequent heel pain. If you are starting to get a little discomfort or pain in the feet or heel, know that pain is not normal. So if you are having pain, you should be proactive and visit our office. If you let heel pain get out of control you could run into several other problems. It is always suggested to visit a podiatrist whenever you are experiencing pain.
What Causes Achilles Tendinitis ?
Overview
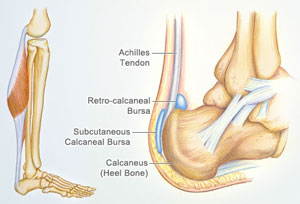
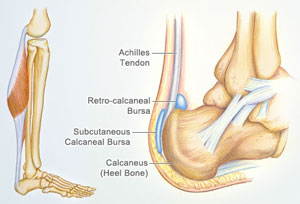
 Achilles tendonitis (tendinitis), is a painful and often debilitating inflammation of the Achilles tendon than can progress into degeneration which we call Achilles Tendinosis. The Achilles tendon is the largest and strongest tendon in the body. It is located in the back of the lower leg, attaches to the heel bone (calcaneus), and connects the calf muscles to the heel bone. In most cases, Achilles tendonopathy's are overuse injuries are more common among athletes and people who train heavily, however it can also occur in people who are less active. Achilles Tendonitis can vary in severity from a mild pain in the tendon during a particular activity to more severe cases when any form of activity that puts strain on this ligament, even standing or walking, can cause pain.
Achilles tendonitis (tendinitis), is a painful and often debilitating inflammation of the Achilles tendon than can progress into degeneration which we call Achilles Tendinosis. The Achilles tendon is the largest and strongest tendon in the body. It is located in the back of the lower leg, attaches to the heel bone (calcaneus), and connects the calf muscles to the heel bone. In most cases, Achilles tendonopathy's are overuse injuries are more common among athletes and people who train heavily, however it can also occur in people who are less active. Achilles Tendonitis can vary in severity from a mild pain in the tendon during a particular activity to more severe cases when any form of activity that puts strain on this ligament, even standing or walking, can cause pain.
Causes
Tight or tired calf muscles, which transfer too much of the force associated with running onto the Achilles tendon. Not stretching the calves properly or a rapid increase in intensity and frequency of sport training can make calf muscles fatigued. Activities which place a lot of stress on the achilles tendon, such as hill running and sprint training, can also cause Achilles Tendinitis. Runners who overpronate (roll too far inward on their feet during impact) are most susceptible to Achilles Tendinitis. Runners with flat feet are susceptible to Achilles Tendinitis because flat feet cause a 'wringing out' effect on the achilles tendon during running. High arched feet usually absorb less shock from the impact of running so that shock is transferred to the Achilles tendon. Use of inappropriate footwear when playing sport or running e.g., sandals, can also put an extra load on the Achilles tendon. Shoes are now available that have been designed for individual sports and provide cushioning to absorb the shock of impact and support for the foot during forceful movements. Training on hard surfaces e.g., concrete, also increases the risk of Achilles Tendinitis. Landing heavily or continuously on a hard surface can send a shock through the body which is partly absorbed by the Achilles tendon. A soft surface like grass turf helps to lessen the shock of the impact by absorbing some of the force of the feet landing heavily on the ground after a jump or during a running motion.
Symptoms
The main complaint associated with Achilles tendonitis is pain behind the heel. The pain is often most prominent in an area about 2-4 centimeters above where the tendon attaches to the heel. In this location, called the watershed zone of the tendon, the blood supply to the tendon makes this area particularly susceptible. Patients with Achilles tendonitis usually experience the most significant pain after periods of inactivity. Therefore patients tend to experience pain after first walking in the morning and when getting up after sitting for long periods of time. Patients will also experience pain while participating in activities, such as when running or jumping. Achilles tendonitis pain associated with exercise is most significant when pushing off or jumping.
Diagnosis
Your physiotherapist or sports doctor can usually confirm the diagnosis of Achilles tendonitis in the clinic. They will base their diagnosis on your history, symptom behaviour and clinical tests. Achilles tendons will often have a painful and prominent lump within the tendon. Further investigations include US scan or MRI. X-rays are of little use in the diagnosis.
Nonsurgical Treatment
Treatment can range from cold compress and heel pads for minor cases, to physical rehabilitation, anti-inflammatory medicine, ultrasound therapy, and manual therapy. If you are a Michigan resident that suspects they have Achilles Tendinitis, please contact Dr. Young immediately; Achilles Tendinitis, if left untreated, can eventually result in an Achilles Tendon Rupture, which is a serious condition that is a partial or complete tear in the tendon. It can severely hinder walking and can be extremely painful and slow to recover.
Surgical Treatment
Surgery should be considered to relieve Achilles tendinitis only if the pain does not improve after 6 months of nonsurgical treatment. The specific type of surgery depends on the location of the tendinitis and the amount of damage to the tendon. Gastrocnemius recession. This is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the Achilles tendon, this procedure is useful for patients who still have difficulty flexing their feet, despite consistent stretching. In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope-an instrument that contains a small camera. Your doctor will discuss the procedure that best meets your needs. Complication rates for gastrocnemius recession are low, but can include nerve damage. Gastrocnemius recession can be performed with or without d?bridement, which is removal of damaged tissue. D?bridement and repair (tendon has less than 50% damage). The goal of this operation is to remove the damaged part of the Achilles tendon. Once the unhealthy portion of the tendon has been removed, the remaining tendon is repaired with sutures, or stitches to complete the repair. In insertional tendinitis, the bone spur is also removed. Repair of the tendon in these instances may require the use of metal or plastic anchors to help hold the Achilles tendon to the heel bone, where it attaches. After d?bridement and repair, most patients are allowed to walk in a removable boot or cast within 2 weeks, although this period depends upon the amount of damage to the tendon. D?bridement with tendon transfer (tendon has greater than 50% damage). In cases where more than 50% of the Achilles tendon is not healthy and requires removal, the remaining portion of the tendon is not strong enough to function alone. To prevent the remaining tendon from rupturing with activity, an Achilles tendon transfer is performed. The tendon that helps the big toe point down is moved to the heel bone to add strength to the damaged tendon. Although this sounds severe, the big toe will still be able to move, and most patients will not notice a change in the way they walk or run. Depending on the extent of damage to the tendon, some patients may not be able to return to competitive sports or running. Recovery. Most patients have good results from surgery. The main factor in surgical recovery is the amount of damage to the tendon. The greater the amount of tendon involved, the longer the recovery period, and the less likely a patient will be able to return to sports activity. Physical therapy is an important part of recovery. Many patients require 12 months of rehabilitation before they are pain-free.
Prevention
Achilles tendinitis cannot always be prevented but the following tips will help you reduce your risk. If you are new to a sport, gradually ramp up your activity level to your desired intensity and duration. If you experience pain while exercising, stop. Avoid strenuous activity that puts excessive stress on your Achilles tendon. If you have a demanding workout planned, warm up slowly and thoroughly. Always exercise in shoes that are in good condition and appropriate for your activity or sport. Be sure to stretch your calf muscles and Achilles tendon before and after working out. If you suffer from Achilles tendinitis make sure you treat it properly and promptly. If self-care techniques don?t work, don?t delay. Book a consultation with a foot care expert or you may find yourself sidelined from your favourite sports and activities.
 Achilles tendonitis (tendinitis), is a painful and often debilitating inflammation of the Achilles tendon than can progress into degeneration which we call Achilles Tendinosis. The Achilles tendon is the largest and strongest tendon in the body. It is located in the back of the lower leg, attaches to the heel bone (calcaneus), and connects the calf muscles to the heel bone. In most cases, Achilles tendonopathy's are overuse injuries are more common among athletes and people who train heavily, however it can also occur in people who are less active. Achilles Tendonitis can vary in severity from a mild pain in the tendon during a particular activity to more severe cases when any form of activity that puts strain on this ligament, even standing or walking, can cause pain.
Achilles tendonitis (tendinitis), is a painful and often debilitating inflammation of the Achilles tendon than can progress into degeneration which we call Achilles Tendinosis. The Achilles tendon is the largest and strongest tendon in the body. It is located in the back of the lower leg, attaches to the heel bone (calcaneus), and connects the calf muscles to the heel bone. In most cases, Achilles tendonopathy's are overuse injuries are more common among athletes and people who train heavily, however it can also occur in people who are less active. Achilles Tendonitis can vary in severity from a mild pain in the tendon during a particular activity to more severe cases when any form of activity that puts strain on this ligament, even standing or walking, can cause pain.
Causes
Tight or tired calf muscles, which transfer too much of the force associated with running onto the Achilles tendon. Not stretching the calves properly or a rapid increase in intensity and frequency of sport training can make calf muscles fatigued. Activities which place a lot of stress on the achilles tendon, such as hill running and sprint training, can also cause Achilles Tendinitis. Runners who overpronate (roll too far inward on their feet during impact) are most susceptible to Achilles Tendinitis. Runners with flat feet are susceptible to Achilles Tendinitis because flat feet cause a 'wringing out' effect on the achilles tendon during running. High arched feet usually absorb less shock from the impact of running so that shock is transferred to the Achilles tendon. Use of inappropriate footwear when playing sport or running e.g., sandals, can also put an extra load on the Achilles tendon. Shoes are now available that have been designed for individual sports and provide cushioning to absorb the shock of impact and support for the foot during forceful movements. Training on hard surfaces e.g., concrete, also increases the risk of Achilles Tendinitis. Landing heavily or continuously on a hard surface can send a shock through the body which is partly absorbed by the Achilles tendon. A soft surface like grass turf helps to lessen the shock of the impact by absorbing some of the force of the feet landing heavily on the ground after a jump or during a running motion.
Symptoms
The main complaint associated with Achilles tendonitis is pain behind the heel. The pain is often most prominent in an area about 2-4 centimeters above where the tendon attaches to the heel. In this location, called the watershed zone of the tendon, the blood supply to the tendon makes this area particularly susceptible. Patients with Achilles tendonitis usually experience the most significant pain after periods of inactivity. Therefore patients tend to experience pain after first walking in the morning and when getting up after sitting for long periods of time. Patients will also experience pain while participating in activities, such as when running or jumping. Achilles tendonitis pain associated with exercise is most significant when pushing off or jumping.
Diagnosis
Your physiotherapist or sports doctor can usually confirm the diagnosis of Achilles tendonitis in the clinic. They will base their diagnosis on your history, symptom behaviour and clinical tests. Achilles tendons will often have a painful and prominent lump within the tendon. Further investigations include US scan or MRI. X-rays are of little use in the diagnosis.
Nonsurgical Treatment
Treatment can range from cold compress and heel pads for minor cases, to physical rehabilitation, anti-inflammatory medicine, ultrasound therapy, and manual therapy. If you are a Michigan resident that suspects they have Achilles Tendinitis, please contact Dr. Young immediately; Achilles Tendinitis, if left untreated, can eventually result in an Achilles Tendon Rupture, which is a serious condition that is a partial or complete tear in the tendon. It can severely hinder walking and can be extremely painful and slow to recover.
Surgical Treatment
Surgery should be considered to relieve Achilles tendinitis only if the pain does not improve after 6 months of nonsurgical treatment. The specific type of surgery depends on the location of the tendinitis and the amount of damage to the tendon. Gastrocnemius recession. This is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the Achilles tendon, this procedure is useful for patients who still have difficulty flexing their feet, despite consistent stretching. In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope-an instrument that contains a small camera. Your doctor will discuss the procedure that best meets your needs. Complication rates for gastrocnemius recession are low, but can include nerve damage. Gastrocnemius recession can be performed with or without d?bridement, which is removal of damaged tissue. D?bridement and repair (tendon has less than 50% damage). The goal of this operation is to remove the damaged part of the Achilles tendon. Once the unhealthy portion of the tendon has been removed, the remaining tendon is repaired with sutures, or stitches to complete the repair. In insertional tendinitis, the bone spur is also removed. Repair of the tendon in these instances may require the use of metal or plastic anchors to help hold the Achilles tendon to the heel bone, where it attaches. After d?bridement and repair, most patients are allowed to walk in a removable boot or cast within 2 weeks, although this period depends upon the amount of damage to the tendon. D?bridement with tendon transfer (tendon has greater than 50% damage). In cases where more than 50% of the Achilles tendon is not healthy and requires removal, the remaining portion of the tendon is not strong enough to function alone. To prevent the remaining tendon from rupturing with activity, an Achilles tendon transfer is performed. The tendon that helps the big toe point down is moved to the heel bone to add strength to the damaged tendon. Although this sounds severe, the big toe will still be able to move, and most patients will not notice a change in the way they walk or run. Depending on the extent of damage to the tendon, some patients may not be able to return to competitive sports or running. Recovery. Most patients have good results from surgery. The main factor in surgical recovery is the amount of damage to the tendon. The greater the amount of tendon involved, the longer the recovery period, and the less likely a patient will be able to return to sports activity. Physical therapy is an important part of recovery. Many patients require 12 months of rehabilitation before they are pain-free.
Prevention
Achilles tendinitis cannot always be prevented but the following tips will help you reduce your risk. If you are new to a sport, gradually ramp up your activity level to your desired intensity and duration. If you experience pain while exercising, stop. Avoid strenuous activity that puts excessive stress on your Achilles tendon. If you have a demanding workout planned, warm up slowly and thoroughly. Always exercise in shoes that are in good condition and appropriate for your activity or sport. Be sure to stretch your calf muscles and Achilles tendon before and after working out. If you suffer from Achilles tendinitis make sure you treat it properly and promptly. If self-care techniques don?t work, don?t delay. Book a consultation with a foot care expert or you may find yourself sidelined from your favourite sports and activities.
What May Cause Heel Discomfort

Overview
The plantar fascia is a thick fibrous band that runs the length of the sole of the foot. The plantar fascia helps maintain the complex arch system of the foot and plays a role in one's balance and the various phases of gait. Injury to this tissue, called plantar fasciitis, is one of the most disabling running injuries and also one of the most difficult to resolve. Plantar fasciitis represents the fourth most common injury to the lower limb and represents 8 -10% of all presenting injuries to sports clinics (Ambrosius 1992, Nike 1989). Rehabilitation can be a long and frustrating process. The use of preventative exercises and early recognition of danger signals are critical in the avoidance of this injury.
Causes
Because the plantar fascia supports your foot and gets used every time you take a step, it has to absorb a large amount of stress and weight. If too much pressure is put on the plantar fascia, the fibers can become damaged or start to tear. The body responds by causing inflammation in the affected area. This is what causes the pain and stiffness of plantar fasciitis. Things that can increase the risk of plantar fasciitis include tight calf muscles. Tight calves make it harder to flex your foot, and this puts more stress on the plantar fascia. Weight. Carrying a few extra pounds puts added pressure on your feet every time you take a step. Activities that put a lot of stress on the feet. This includes things like running, hiking, dancing, and aerobics. Bad shoes. Footwear that doesn't give your foot the support it needs increases your risk of plantar fasciitis. You'll want to ditch any shoes that have thin soles or inadequate arch support, or ones that don't fit your feet properly. Routinely wearing high heels can also cause your Achilles tendon to contract over time, making it harder to flex your foot. Jobs that involve a lot of standing or walking on hard surfaces. Jobs that keep you on your feet all day, like waiting tables or working in a store, can cause damage to your plantar fascia. High arches, flat feet, or other foot problems. The shape of your foot can affect the way your weight is distributed on your feet when you stand. If weight distribution is a bit off, it can add to a person's risk of plantar fasciitis. How someone walks can increase the stress on certain parts of the foot too.
Symptoms
If you have Plantar Fasciitis, you will most likely feel a sharp pain under the ball of you heel and it will often give pain when standing after a period of rest. For example when you get out of bed in the mornings or after being sat down. Some patients describe this feeling as a stone bruise sensation, or a pebble in the shoe and at times the pain can be excruciating. Patients with Plantar Fasciitis can experience pain free periods whereby the think they are on the mend, only for the heel pain to come back aggressively when they appear to have done nothing wrong. If your plantar fasciitis came on very suddenly and the pain is relentless, then you may have Plantar Fascial Tears. We will be able to differentiate between these 2 conditions, sometimes with ultra sound imaging. The treatment for each of these conditions will need to be very different.
Diagnosis
Your GP or podiatrist (a healthcare professional who specialises in foot care) may be able to diagnose the cause of your heel pain by asking about your symptoms and examining your heel and foot. You will usually only need further tests if you have additional symptoms that suggest the cause of your heel pain is not inflammation, such as numbness or a tingling sensation in your foot, this could be a sign of nerve damage in your feet and legs (peripheral neuropathy) your foot feels hot and you have a high temperature (fever) of 38C (100.4F) or above - these could be signs of a bone infection, you have stiffness and swelling in your heel, this could be a sign of arthritis. Possible further tests may include blood tests, X-rays - where small doses of radiation are used to detect problems with your bones and tissues, a magnetic resonance imaging (MRI) scan or ultrasound scan, which are more detailed scans.
Non Surgical Treatment
The good news is that plantar fasciitis is reversible and very successfully treated. About 90 percent of people with plantar fasciitis improve significantly within two months of initial treatment. If your plantar fasciitis continues after a few months of conservative treatment, your doctor may inject your heel with steroidal anti-inflammatory medications (corticosteroid). Cortisone injections have been shown to have short-term benefits but they actually retard your progress in the medium to long-term, which usually means that you will suffer recurrent bouts for longer. Due to poor foot biomechanics being the primary cause of your plantar fasciitis it is vital to thoroughly assess and correct your foot and leg biomechanics to prevent future plantar fasciitis episodes or the development of a heel spur. Your physiotherapist is an expert in foot assessment and its dynamic biomechanical correction. They may recommend that you seek the advice of a podiatrist, who is an expert in the prescription on passive foot devices such as orthotics.

Surgical Treatment
When more conservative methods have failed to reduce plantar fasciitis pain, your doctor may suggest extracorporeal shock wave therapy, which is used to treat chronic plantar fasciitis. Extracorporeal shock wave therapy uses sound waves to stimulate healing, but may cause bruises, numbness, tingling, swelling, and pain. When all else fails, surgery may be recommended to detach the plantar fascia from the heel bone. Few people need surgery to treat the condition.
Prevention
Every time your foot strikes the ground, the plantar fascia is stretched. You can reduce the strain and stress on the plantar fascia by following these simple instructions: Avoid running on hard or uneven ground, lose any excess weight, and wear shoes and orthotics that support your arch to prevent over-stretching of the plantar fascia.
What Can Cause Pain In The Heel And The Ways To Treat It
Overview
Plantar fasciitis is a very common condition resulting in pain under the heel which often radiates into the foot. We explain free of charge everything you need to know to cure your pain and prevent it from returning.
Causes
This is a problem of either extreme, so people with high arches or those that have very flat feet are at risk of developing pain in this region. This is because of the relative stress the plantar fascia is put under. In people with excessive pronation, the plantar fascia is put under too much stretch, as their range flattens and strains it. People with a stiff, supinated (high-arched) foot lack the flexibility to appropriately shock absorb, so this too puts extra strain on the plantar fascia. Clinically, we see more people presenting with plantar fascia pain who have excessive pronation than those with stiff, supinated feet. But while the foot type is the biggest risk factor for plantar fasciitis, the whole leg from the pelvis down can affect how the foot hits the ground. A thorough biomechanical assessment will determine where in the kinetic chain things have gone wrong to cause the overload.
Symptoms
A very common complaint of plantar fasciitis is pain in the bottom of the heel. Plantar fasciitis is usually worse in the morning and may improve throughout the day. By the end of the day the pain may be replaced by a dull aching that improves with rest. Most people suffering from plantar fasciitis also complain of increased heel pain after walking for a long period of time.
Diagnosis
A health care professional will ask you whether you have the classic symptoms of first-step pain and about your activities, including whether you recently have intensified your training or changed your exercise pattern. Your doctor often can diagnose plantar fasciitis based on your history and symptoms, together with a physical examination. If the diagnosis is in doubt, your doctor may order a foot X-ray, bone scan or nerve conduction studies to rule out another condition, such as a stress fracture or nerve problem.
Non Surgical Treatment
Plantar fasciitis is usually controlled with conservative treatment. Following control of the pain and inflammation an orthotic (a custom made shoe insert) will be used to stabilize your foot and prevent a recurrence. Over 98% of the time heel spurs and plantar fasciitis can be controlled by this treatment and surgery can be avoided. The orthotic prevents excess pronation and prevents lengthening of the plantar fascia and continued tearing of the fascia. Usually a slight heel lift and a firm shank in the shoe will also help to reduce the severity of this problem. The office visit will be used for careful examination and review to distinguish plantar fasciitis and plantar heel pain syndrome from other problems, many of which are outlined below. It is important to distinguish between a stress reaction of the calcaneus and plantar fasciitis. A feature of many calcaneal stress fractures is pain on lateral and medial compression of the calcaneus.

Surgical Treatment
The most common surgical procedure for plantar fasciitis is plantar fascia release. It involves surgical removal of a part from the plantar fascia ligament which will relieve the inflammation and reduce the tension. Plantar fascia release is either an open surgery or endoscopic surgery (insertion of special surgical instruments through small incisions). While both methods are performed under local anesthesia the open procedure may take more time to recover. Other surgical procedures can be used as well but they are rarely an option. Complications of plantar fasciitis surgery are rare but they are not impossible. All types of plantar fasciitis surgery pose a risk of infection, nerve damage, and anesthesia related complications including systemic toxicity, and persistence or worsening of heel pain.
Prevention
The following steps will help prevent plantar fasciitis or help keep the condition from getting worse if you already have it. Take care of your feet. Wear shoes with good arch support and heel cushioning. If your work requires you to stand on hard surfaces, stand on a thick rubber mat to reduce stress on your feet. Do exercises to stretch the Achilles tendon at the back of the heel. This is especially important before sports, but it is helpful for non-athletes as well. Ask your doctor about recommendations for a stretching routine. Stay at a healthy weight for your height. Establish good exercise habits. Increase your exercise levels gradually, and wear supportive shoes. If you run, alternate running with other sports that will not cause heel pain. Put on supportive shoes as soon as you get out of bed. Going barefoot or wearing slippers puts stress on your feet. If you feel that work activities caused your heel pain, ask your human resources department for information about different ways of doing your job that will not make your heel pain worse. If you are involved in sports, you may want to consult a sports training specialist for training and conditioning programs to prevent plantar fasciitis from recurring.
What Is Heel Discomfort

Overview
Plantar fasciitis is a common cause of heel pain in adults. The pain is usually caused by collagen degeneration (which is sometimes misnamed “chronic inflammation”) at the origin of the plantar fascia at the medial tubercle of the calcaneus. This degeneration is similar to the chronic necrosis of tendonosis, which features loss of collagen continuity, increases in ground substance (matrix of connective tissue) and vascularity, and the presence of fibro-blasts rather than the inflammatory cells usually seen with the acute inflammation of tendonitis. The cause of the degeneration is repetitive microtears of the plantar fascia that overcome the body's ability to repair itself.
Causes
Excessive stretching of the plantar fascia can result in microtrauma of this structure either along its course or where it inserts onto the medial calcaneal tuberosity. This microtrauma, if repetitive, can result in chronic degeneration of the plantar fascia fibers. The loading of the degenerative and healing tissue at the plantar fascia may cause significant plantar pain, particularly with the first few steps after sleep or other periods of inactivity. The term fasciitis may, in fact, be something of a misnomer, because the disease is actually a degenerative process that occurs with or without inflammatory changes, which may include fibroblastic proliferation. This has been proven from biopsies of fascia from people undergoing surgery for plantar fascia release.
Symptoms
Pain tends to start gradually, often just in the heel, but it can sometimes be felt along the whole of the plantar fascia. The symptoms are initially worse in the morning and mostly after, rather than during, activity. As the condition becomes worse, the symptoms become more persistent.
Diagnosis
To diagnose plantar fasciitis, your doctor will physically examine your foot by testing your reflexes, balance, coordination, muscle strength, and muscle tone. Your doctor may also advise a magnetic resonance imaging (MRI) or X-ray to rule out other others sources of your pain, such as a pinched nerve, stress fracture, or bone spur.
Non Surgical Treatment
Heel cups are used to decrease the impact on the calcaneus and to theoretically decrease the tension on the plantar fascia by elevating the heel on a soft cushion. Although heel cups have been found to be useful by some physicians and patients, in our experience they are more useful in treating patients with fat pad syndrome and heel bruises than patients with plantar fasciitis. In a survey of 411 patients with plantar fasciitis, heel cups were ranked as the least effective of 11 different treatments.

Surgical Treatment
The most common surgical procedure for plantar fasciitis is plantar fascia release. It involves surgical removal of a part from the plantar fascia ligament which will relieve the inflammation and reduce the tension. Plantar fascia release is either an open surgery or endoscopic surgery (insertion of special surgical instruments through small incisions). While both methods are performed under local anesthesia the open procedure may take more time to recover. Other surgical procedures can be used as well but they are rarely an option. Complications of plantar fasciitis surgery are rare but they are not impossible. All types of plantar fasciitis surgery pose a risk of infection, nerve damage, and anesthesia related complications including systemic toxicity, and persistence or worsening of heel pain.
Exercises For Plantar Warts
Pain across the bottom of the foot at any point between the heel and the ball of the foot is often referred to as "arch pain” Although this description is non-specific, most arch pain is due to strain or inflammation Mallet Toe of the plantar fascia (a long ligament on the bottom of the foot). Wearing inappropriate footwear or foot problems like athlete's foot and Morton's neuroma are some of the factors that cause burning feet sensation.
If changing your shoes isn't helping to solve your foot pain, it is time for us to step in. Contact Dr. Jeff Bowman at Houston Foot Specialists for treatment that will keep your feet feeling great. Inserting arch support insoles in the shoes is also a good option.
If you see just a thin line connecting the ball of your foot to your heel, you have high arches. If you have flat feet or high arches, you're more likely to get plantar fasciitis, an inflammation of the tissue along the bottom of your foot. Without proper arch support, you can have pain in your heels, arch, and leg. You can also develop bunions and hammertoes, which can become painful,” says Marlene Reid, a podiatrist, or foot and ankle doctor, in Naperville, IL. Shoes with good arch support and a slightly raised heel can help ward off trouble. Laces, buckles, or straps are best for high arches. See a foot doctor to get fitted with custom inserts for your shoes. Good running shoes, for example, can prevent heel pain, stress fractures , and other foot problems that can be brought on by running. A 2-inch heel is less damaging than a 4-inch heel. If you have flat feet, opt for chunky heels instead of skinny ones, Reid says.
Do not consume food items which you are allergic to. Keep dead skin off your lips by lightly scrubbing them at least twice a week using a mild, natural ingredient such as cornflour or a lemon juice-sugar pack. I had a long road workout two weeks ago and immediately after starting having pain on the ball of my foot in this area. I have also learned buying shoes online is easy.
During the average lifetime our feet cover over 70,000 miles, the equivalent of walking four times around the world., so it's not surprising that problems can occur. Indeed around three-quarters of all adults will experience some sort of problem with their feet at some time. And without treatment most foot complaints will become gradually worse with time. This means people often endure painful conditions for far too long, and the problem can get worse. People often assume nothing can be done to help their condition, but in fact these conditions are extremely treatable. Swollen lump on big toe joint; lump may become numb but also make walking painful.
If changing your shoes isn't helping to solve your foot pain, it is time for us to step in. Contact Dr. Jeff Bowman at Houston Foot Specialists for treatment that will keep your feet feeling great. Inserting arch support insoles in the shoes is also a good option.
If you see just a thin line connecting the ball of your foot to your heel, you have high arches. If you have flat feet or high arches, you're more likely to get plantar fasciitis, an inflammation of the tissue along the bottom of your foot. Without proper arch support, you can have pain in your heels, arch, and leg. You can also develop bunions and hammertoes, which can become painful,” says Marlene Reid, a podiatrist, or foot and ankle doctor, in Naperville, IL. Shoes with good arch support and a slightly raised heel can help ward off trouble. Laces, buckles, or straps are best for high arches. See a foot doctor to get fitted with custom inserts for your shoes. Good running shoes, for example, can prevent heel pain, stress fractures , and other foot problems that can be brought on by running. A 2-inch heel is less damaging than a 4-inch heel. If you have flat feet, opt for chunky heels instead of skinny ones, Reid says.

Do not consume food items which you are allergic to. Keep dead skin off your lips by lightly scrubbing them at least twice a week using a mild, natural ingredient such as cornflour or a lemon juice-sugar pack. I had a long road workout two weeks ago and immediately after starting having pain on the ball of my foot in this area. I have also learned buying shoes online is easy.

During the average lifetime our feet cover over 70,000 miles, the equivalent of walking four times around the world., so it's not surprising that problems can occur. Indeed around three-quarters of all adults will experience some sort of problem with their feet at some time. And without treatment most foot complaints will become gradually worse with time. This means people often endure painful conditions for far too long, and the problem can get worse. People often assume nothing can be done to help their condition, but in fact these conditions are extremely treatable. Swollen lump on big toe joint; lump may become numb but also make walking painful.
Learn About Feet
Elderly individuals (can be called geriatric) are susceptible to a number of foot specific conditions Some of these conditions can leave individuals disabled if they are not prevented and/or taken care of. Some of these common foot related conditions include: arthritis, ingrown toenails, fungal nails, diabetic ulcers, and corns/calluses. It is an interesting fact that if you were to go barefoot every day of your life, you would not suffer with feet corns.
Hand, foot and mouth disease is usually spread from person- to -person through faecal contamination (which can occur when changing a nappy or using the toilet and not properly washing hands afterwards), or spread through respiratory secretions (saliva, sputum, or nasal mucus) of an infected person. There is no clear evidence of risk to unborn babies from hand, foot and mouth disease. However, infected mothers can pass the infection onto newborn babies who rarely can have severe disease. Avoid sharing cups, eating utensils, items of personal hygiene (for example: towels, washers and toothbrushes), and clothing (especially shoes and socks). Children with hand, foot and mouth disease should be excluded from school or childcare facilities until their blisters have dried. Thus it helps loosen the hard and scaly skin.
There are four major stages with which pain will begin in our body. The first is the actual stimulus, which starts the pain information pathway to the brain. Before the electrical information finally enters the brain, the body has a third step in the pain route, called modulation. Once the brain accepts the electrical signal and final process begins, which is the awareness of pain in the body. The two main goals that a podiatrist wants to achieve in treating pain are to eliminate the source of the problem and also to treat the symptoms caused by the problem. In order to do so, the podiatrist will need to investigate the cause of the pain by first asking the patient a series of questions regarding the problem. There are different types of pain in the body. If the pain is tingling or burning, the problem is most probably associated with the nerve.
Most cases of foot pain can be treated without surgery, whether it's metatarsal foot pain, ball-of-foot pain, foot arch pain or some other type. At the start to notice soreness or discomforts around the foot area, it is imperative to take rest, put on or apply cold or ice compress, and or elevate the affected foot. Generally, foot pains vary from mild to severe. However, prevention is above all better than to deal with any pain though. Never take for granted to any pain; focus on getting foot pain reliever at the soonest is vital. In case the pain is unbearable which it hampers the usual life activities, it is imperative to look for urgent medical or therapist to help and also consider the ordinary methods to lessen foot pain. Stretching exercises also facilitate to soothe the muscles on the feet and help out in the contraction of the muscles. Not all skin disorders respond to treatment.
When a patient suffers a foot or lower leg injury they should see a podiatrist as soon as possible to receive the appropriate advice and treatment. The podiatrist will need to understand the cause of the injury, any previous injuries and the level of activity prior to the injury occurring. A comprehensive biomechanical assessment of the patient walking or running will then be carried out to outline any issues with foot/knee or hip alignment that may be causing or contributing to the condition. Podiatrists care for any skin and nail problem involving the feet. The skin may turn red, and start peeling.
Footwear can be modified with stretching over the protruded area to further reduce pressure and in extreme cases footwear can be modified with a balloon patch. In this case, the Pedorthist would cut a hole in the upper of the shoe at the bunion area and place a patch over the hole to create more space for the bunion. Orthotics in this case can help to bring the foot into a more neutral position therefore reducing pressure on the joint and resulting pain. It should be noted that orthotics should always be put into proper fitting footwear to achieve the best results. Proper footwear is the first step in the treatment of a neuroma.
Wear shoes that fit your feet well and allow your toes to move. After years of neuropathy, as reflexes are lost, the feet are likely to become wider and flatter. Cover your feet (except for the skin between the toes) with petroleum jelly, a lotion containing lanolin, or cold cream before putting on shoes and socks. For persons with diabetes, the feet tend to sweat less than normal.
Hand, foot and mouth disease is usually spread from person- to -person through faecal contamination (which can occur when changing a nappy or using the toilet and not properly washing hands afterwards), or spread through respiratory secretions (saliva, sputum, or nasal mucus) of an infected person. There is no clear evidence of risk to unborn babies from hand, foot and mouth disease. However, infected mothers can pass the infection onto newborn babies who rarely can have severe disease. Avoid sharing cups, eating utensils, items of personal hygiene (for example: towels, washers and toothbrushes), and clothing (especially shoes and socks). Children with hand, foot and mouth disease should be excluded from school or childcare facilities until their blisters have dried. Thus it helps loosen the hard and scaly skin.
There are four major stages with which pain will begin in our body. The first is the actual stimulus, which starts the pain information pathway to the brain. Before the electrical information finally enters the brain, the body has a third step in the pain route, called modulation. Once the brain accepts the electrical signal and final process begins, which is the awareness of pain in the body. The two main goals that a podiatrist wants to achieve in treating pain are to eliminate the source of the problem and also to treat the symptoms caused by the problem. In order to do so, the podiatrist will need to investigate the cause of the pain by first asking the patient a series of questions regarding the problem. There are different types of pain in the body. If the pain is tingling or burning, the problem is most probably associated with the nerve.
Most cases of foot pain can be treated without surgery, whether it's metatarsal foot pain, ball-of-foot pain, foot arch pain or some other type. At the start to notice soreness or discomforts around the foot area, it is imperative to take rest, put on or apply cold or ice compress, and or elevate the affected foot. Generally, foot pains vary from mild to severe. However, prevention is above all better than to deal with any pain though. Never take for granted to any pain; focus on getting foot pain reliever at the soonest is vital. In case the pain is unbearable which it hampers the usual life activities, it is imperative to look for urgent medical or therapist to help and also consider the ordinary methods to lessen foot pain. Stretching exercises also facilitate to soothe the muscles on the feet and help out in the contraction of the muscles. Not all skin disorders respond to treatment.
When a patient suffers a foot or lower leg injury they should see a podiatrist as soon as possible to receive the appropriate advice and treatment. The podiatrist will need to understand the cause of the injury, any previous injuries and the level of activity prior to the injury occurring. A comprehensive biomechanical assessment of the patient walking or running will then be carried out to outline any issues with foot/knee or hip alignment that may be causing or contributing to the condition. Podiatrists care for any skin and nail problem involving the feet. The skin may turn red, and start peeling.
Footwear can be modified with stretching over the protruded area to further reduce pressure and in extreme cases footwear can be modified with a balloon patch. In this case, the Pedorthist would cut a hole in the upper of the shoe at the bunion area and place a patch over the hole to create more space for the bunion. Orthotics in this case can help to bring the foot into a more neutral position therefore reducing pressure on the joint and resulting pain. It should be noted that orthotics should always be put into proper fitting footwear to achieve the best results. Proper footwear is the first step in the treatment of a neuroma.
Wear shoes that fit your feet well and allow your toes to move. After years of neuropathy, as reflexes are lost, the feet are likely to become wider and flatter. Cover your feet (except for the skin between the toes) with petroleum jelly, a lotion containing lanolin, or cold cream before putting on shoes and socks. For persons with diabetes, the feet tend to sweat less than normal.
